What is Ovarian Cancer
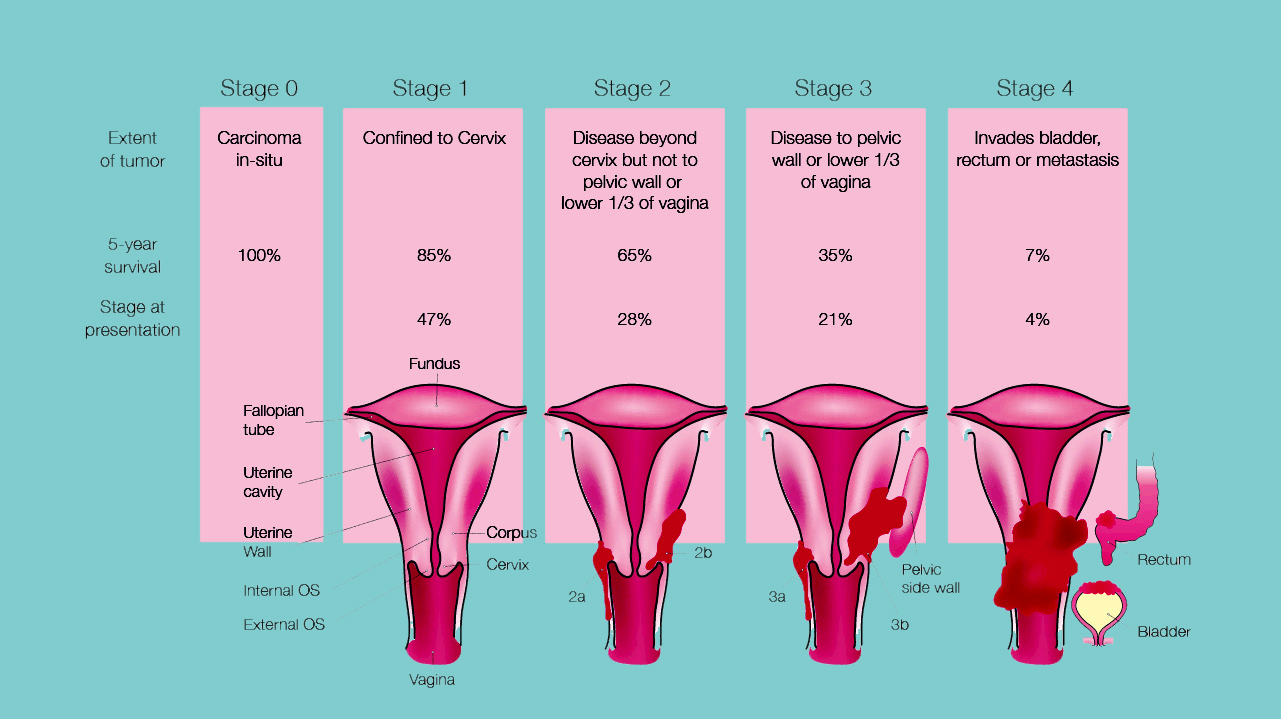
Our body is constantly producing new cells to allow us to grow and replace old or injured cells. These cells usually grow in a predictable and organized way. But sometimes cells behave and grow abnormally and form a growth or lump called a 'tumor'. The ovaries are two small (about 2–4 cm) almond shaped organs that are part of the female reproductive system. They sit on either side of the uterus (womb). Other parts of the female reproductive system include the fallopian tubes, cervix and vagina. Each ovary contains germ cells that eventually develop into eggs (ova). In women who are having periods, a mature egg is released by the ovary each month (this is called 'ovulation'). Your ovaries also produce the hormones oestrogen and progesterone, which regulate your menstrual cycle and affect the development of female body characteristics – such as breasts, body hair and body shape. Ovarian cancer is a general term used to describe a cancerous (malignant) tumor starting in one or both ovaries. The ovaries are made up of three main kinds of cells – epithelial cells, stromal cells and germ cells. Each of these cells can develop into a different type of tumor. The average age of women when they are diagnosed with ovarian cancer is age 64. It is mainly diagnosed in women over the age of 50; however, there are cases diagnosed in younger women.